How to manage Interstitial Cystitis/Bladder Pain Syndrome?
March 26, 2017, 3 responses, by: Women Health Center, Tags: interstitial cystitis causes, interstitial cystitis diagnosis, interstitial cystitis treatment
Abstract and Introduction
Abstract
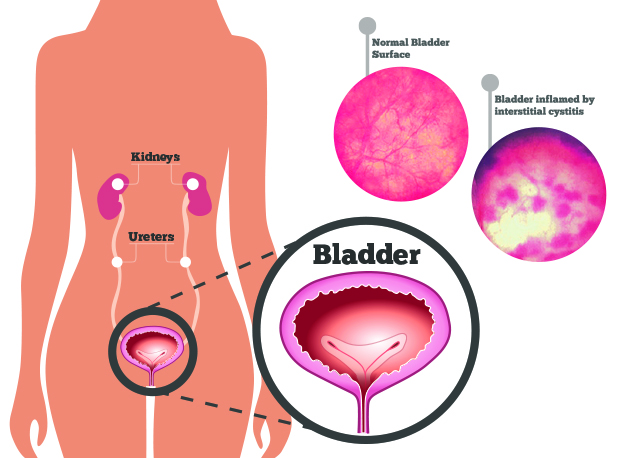
Interstitial cystitis (IC) also called as bladder pain syndrome (BPS) is a chronic bladder health condition causing pain or discomfort in the bladder area in the non-appearance of infection and other identifiable causes. The precise etiology of Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS) is not known, which leads to complications in its treatment. It has however been frequently found in patients with endometriosis and may be responsible for the bladder symptoms encountered in patients with no obvious endometriosis in the bladder.
The American Urological Association (AUA) guidelines suggested a stepwise outlook to the selection of treatment options on the basis of severity of symptoms and characteristics of the patient. Because the experts are not able to fully understand this problem, the aim of the therapy is to provide relief from its symptoms and better quality of life. However, in some patients its symptoms may come and go while for others, they are persistent.
Introduction
Interstitial cystitis and bladder pain syndrome or painful bladder syndrome represents a chronic health disorder which involves a feeling of pain and pressure in the bladder and significantly affect the quality of life. Chronic discomfort or pain in bladder area is referred to as Interstitial cystitis (IC), but, as physicians have no clear understanding about the cause of bladder inflammation (cystitis). There is no evidence that inflammation of the bladder is related to abnormalities of the interstices of the bladder or the pathophysiology.
The term BPS is not used without IC because the previous efforts identify IC as a medical condition with debilitating effects, so for progressive reasons it is called IC/BPS.
Background
There is no clear consensus for the optimal treatment of complications associated with the management of IC/BPS. Different patients suffer from different symptoms of (IC/BPS), depending on the condition and the treatment related to the outcomes may vary from patient to patient as well. There is also a lack of randomized and controlled treatments. The IC/BPS is defined as an unpleasant sensation (discomfort, pain and pressure) perceived to be associated with the urinary bladder and with lower urinary tract symptoms, according to the American Urological Association (AUA).
The estimated commonness of IC/BPS may vary on the basis of the method used. It is more common in women and recent studies shows that female-to-male ratio to be 10:1. In the United States, the estimated commonness is 2.7% – 6.53% among the adult women. This condition is also seen in patients with other painful disorder like fibromyalgia, irritable bowel syndrome or allergies.
The findings published by the National Institutes of Health’s (NIH) 2012, in America stated that the annual expenditure of Urological Diseases exclusive of medication fees is $249,160,233 for Medicare beneficiaries who are below or equals to 65 years old.
I would suggest using diagnostic criteria to identify the condition as a treatment approach to IC/BPS. It is also recommend that one adopts a stepwise method to help in selecting the most effective therapeutic option, depending on the severity of symptoms and characteristics in each individual patient. The AUA has also stated guidelines on the diagnosis and management of IC/BPS. However, they also specified that the guidelines should not be interpreted rigidly.
Pathogenesis
Although there is no clear evidence to understand the aetiology and pathogenesis of IC/BPS, but there may be various factors that cause manifestation of this disease and various different mechanisms have been also proposed.
In cases of IC/BPS many urothelial abnormalities have been found like an autoimmune or immunologic response leading to altered bladder epithelial expression of specific antigens, changes in the glycosaminoglycan (GAG) layer, and altered cytokeratin profile. The GAG layer aids in protecting the bladder from surface irritant, so if it is changed the irritants may leak into the bladder tissue from the urine, which in turn causes inflammation and pain. The bladder wall is also scarred, sometimes or show petechial hemorrhages referred as glomerulations. The hunner lesions or patches of broken skin on the bladder wall are seen in about 10% of IC/BPS cases.
Some findings also recommends that foods and beverages like spicy foods, citrus fruits, alcohol, caffeine and tomatoes may make the symptoms more severe from patient to patient.
It has also been associated with endometriosis where there is no obvious bladder endometriosis and once again is thought to be due to an immunologic response.
Symptoms
The symptoms of Interstitial Cystitis may vary from person to person, how the most common symptoms are excessive discomfort or pain when the bladder fills and relief after urinating. Other symptoms that often appear in patients are nocturia, urinary urgency, frequent urination in daytime, painful urination, perineal pain, pressure in pubic areas, gross hematuria, sensation of bladder spasms, suprapubic pain, depression and dyspareunia. Most of the patients experience poor quality of life and a disruption of work and home activities during this condition.
Diagnosis
The diagnostic criteria involve collection of patient’s history of symptoms as well as related conditions after which a physical investigation and urine testing is done. Cystoscopy can be conducted to exclude other aetiologies, but this is not essential to diagnose IC/BPS. It should be performed only if patients are experiencing haematuria or to identify and understand other conditions. It can be also conducted to identify the structural lesions and intravesical foreign body which helps in identifying a small subgroup of patients that may be treated with cystoscopic treatment.
The validated scales have been developed to assess the severity of IC/BPS and clinical progress, but they do not aid in distinguishing it from other conditions. There have been many scales that are used to assess IC/BPS such the Pelvic pain, the Genitourinary Pain Index, the pelvic pain, Urgency/Frequency (PUF), and IC Symptom and Problem Index questionnaire.
However, haematuria and infection must be excluded so urine analysis must be performed by using microscopy in all the patients that are suspected to be affected with IC/BPS. Also a post void urine test should be also conducted which will help in assessing the urination problems.
Interstitial Cystitis Treatment Options
Since physicians have not understood the aetiology and pathogenesis of IC/BPS, there is no curative treatment available for it. However, they always aim to provide great relief from its associated symptoms so as to provide a good quality of life. The Data Base drawn from the studies state that there is no effective treatment that can provide consistent relief. The analysis was done on 581 women who underwent 183 different types of treatment in the follow up period of IC/BPS and in majority of investigations no particular therapy was successful for the participants.
There is a stepwise approach used for the treatment of IC/BPS and the treatments are identified and selected on the basis of risk of adverse effects and invasiveness of the diseases. The approach of management is organized in a way of increasing risk and when the approach appears to be ineffective, the clinicians should move from one level to the next.
First Line
The initial treatment should be done on the basis of severity of the symptom, patient preferences and clinical judgements. The patients must be also counselled on reasonable expectations for the treatment results. The options available in First-line treatment are patients behavioural modification, education, general relaxation, pain management and stress management.
Patient information on normal bladder function, what is known and not known about the IC/BPS condition, associated risks and the treatment options available. But no single agent has found any effective outcomes in the majority of patients and patient acceptable symptom control may need trials for several options including combination therapy.
Additionally, self-care practices and behavioural modifications are also important educational topics. These may also include fluid restriction or increasing the hydration to alter the concentration of urine, application of local heat or cold over the Perineum or bladder, taking a restricted diet to determine the foods that may increase the risks, avoid taking foods that are known to be irritants, bladder training, using OTC products (including Nutraceuticals, Pyridium, calcium glycerophosphate), pelvic floor muscle relaxation and mind and body strategies to pain flare ups (like meditation, imagery).
According to National Institute of Diabetes and Digestive and Kidney Diseases (NIDKK) that aim in the treatment of IC/BPS patients, the strategies given above have proven to be very effective. In this trial, patients completed a standardized education and behavioural modification program (EBMP). About 45% of patients assigned to the EBMP with placebo group were moderately improved on the global response assessment.
Other First line treatment options include stress management and relaxation. Acupuncture, yoga and hypnosis have been also used with different outcomes.
Second-line
The options available for second-line treatment consist of appropriate manual physical therapy methods such as oral medications which includes pentosan polysulfate sodium (PPS), cimetidine, amitriptyline or hydroxyzine. There are also intervesical therapies like heparin, or lidocaine, pain management and dimethylsulfoxide (DMSO).
Cimetidine
Cimetitide is a histamine receptor antagonist (H2RA) and it is found to be statistically significant to placebo for improving overall symptoms of nocturia or pain, when consumed 400 mg 2 times daily. There were other observational investigations also on the basis of 300 mg twice daily or 200 mg 3-times daily, which results in 44%-57% of patients reported to have gone through significant improvement in symptoms.
Amitriptyline
A randomized controlled trial reported that amitriptyline, a tricyclic antidepressant (TCA) is an effective placebo when its dosage being titrated from 325mg-100mg regularly over various weeks as suggested. It clinically showed a significant relief from pain and intensity of urgency in contrast to placebo (P<.001). The most general and adverse effects in this condition were anticholinergic in nature (e.g. Nausea, sedation and drowsiness) and were seen in 92% of patients in this group and 21% in the placebo group. However, TCA should be started with a low dose and titrated slowly when used for treatment of IC/BPS.
Pain management
The treatment options for pain management must be continually valuated because reducing pain, enhance the quality of life. However, if pain is not controlled, then a multidisciplinary outlook should be chosen. A pain regimen with breakthrough pain management strategies should be considered, if patients experience treatment flares. They focus to design a pain regimen that provides great relief without any side-effects. Urinary analgesics, nonsteroidal anti-inflammatory drugs (NSAIDs), narcotics, aspirin, and various non-narcotic agents can be used to treat chronic pain. Urinary analgesics include methenamine and phenazopyridine. These should not be used for long-term as it may cause liver or renal dysfunction. Intravesical lidocaine with sodium bicarbonate or heparin may be also used for those affected with severe bladder pain. As it requires bladder catherization and should be only used in patients that have had enough relief from other agents.
Hydroxine
According to findings of randomized controlled trial about 23% of patients were treated and experienced clinically significant improvement in urgency and pain in contrast to 13% of patients that were treated in placebo group for a 6 month period. Patients that took 10 mg daily and titrated to 50-mg daily. According to observational study patients that were started on 25 mg, hydroxyzine daily and titrated to 75 mg daily. This study also showed that 92% of patients experienced relief in urinary symptoms. Most importantly, the patients in this investigation had systemic allergies, which may have caused due to hydroxyzine. However, adverse events were common in both the observations and were not serious on an overall basis.
Clinicians recommend that patients with insomnia should take hydroxyzine at bedtime in order to avoid frequent urination at night. However, its hypnotic effect may be helpful for these patients.
PPS
Pentosan polysulfate sodium (PPS, Elmiron) is the most studied and effective drugs for the treatment of IC/BPS and it is available under the brand name Elmiron. It is the only medicine that FDA has approved for the treatment of Bladder pain or discomfort related to IC/BPS. It has fibrinlytic and anticoagulant characteristics and helps to control cell permeability as it represent the mucosal memberane of the bladder wall. This prevents the irritating solutes in the urine from reaching the cells in the lining of the bladder. According to the AUA guideline, PSS is considered to be higher grade because of a large number of observations.
It must be noted that the trials were fairly high quality, but showed mixed outcomes. For instance, in a randomized, placebo controlled study, 38% of patients which were about 155 in number and took 100 mg 3-times in a day for a period of 3 months and 18% of patients who received placebo reported >50% relief in bladder pain.
Another randomized controlled trial conducted on patients who took 200mg 2-times daily for 4 months, but there is no significant difference in overall symptom scores. The suggested dosage of PPS is 100 mg 3-times daily and it may take 3-6 months for symptom relief. PPS is suggested to be an effective treatment for patients who have sedation with antihistamines.
Intravesical Treatments
Intravesical drug installations which consist of Heparin, lidocaine, DMSO is the second-line treatment option according to the AUA guidelines. Intravesical administration of bladder provides a large concentration of medication to the target area and leads to very less systemic side effects. The limitations associated with this method include risk factors, cost and pain caused from intermittent catheterization.
FDA has approved DMSO as the only drug for installation of intravesical drug. As this treatment is considered to provide great relief by having analgesic, anti-inflammatory, mast-cell inhibition and smooth muscle relaxation. It is usually given as a cocktail that may consist of sodium bicarbonate, heparin, lidocaine and a local steroid preparation. First a catheter is placed in the bladder and then, DMSO is passed through it and held for 10-15 minutes prior to normal voiding. This treatment is generally given every 1-2 weeks for 6-8 weeks and repeated as per individual need.
Third- to Sixth-line
In case the first and second line treatments have not helped the patients with worsening symptoms, then you must consider a third-line treatment. Thirdline treatments include cystoscopy under anesthesia with short duration, pain management, low-pressure hydrodistention and treatment of Hunner lesions. The options available for fourth-line treatment include botulinum toxin A (Botox) injections into the muscles of the bladder, neuromodulation, and pain management.
Botox can lead to many adverse effects like painful urination and painful urination. Although Neurostimulation may not provide much relief from pain but may be useful for urinary frequency. Fifth-line treatments include cyclosporine A with pain management and sixth-line treatments include various options such as diversions with or without cystectomy, substitution cystoplasty and pain management.
In Menopausal patients Hormone replacement therapy has also been useful. The Mona Lisa Touch treatment is also being investigated as an alternative treatment option in these patients.
Synopsis
Even though it is challenging to treat IC/BPS due to lack of data and lack of consistency in the symptoms experienced. The AUA guideline provides a starting point for management, but the treatment should be given according to individual preference of each patient. The treatment should comprise of both nonpharmacologic and pharmacologic and a stepwise approach must be followed.
3 responses to “How to manage Interstitial Cystitis/Bladder Pain Syndrome?”
Leave a Reply
Categories
- Endometriosis (3)
- Female Sexual dysfunction (1)
- General (7)
- Incontinence (1)
- Infertility (2)
- Interstitial Cystitis (1)
- Menopause (5)
- Overactive Bladder (1)
- Polycystic Ovaries (1)
- Surgical (2)
Archives
- October 2017 (2)
- March 2017 (1)
- March 2016 (1)
- February 2016 (1)
- November 2015 (3)
- October 2015 (5)
- September 2015 (1)
- August 2015 (2)
- July 2015 (3)
- March 2015 (2)
- January 2015 (1)
Recent Posts
- How Accurate is biopsy sampling in Endometrial Cancer?
- Hormone Therapy: WHI study Follow up reveals no change in Mortality after 18-Year
- How to manage Interstitial Cystitis/Bladder Pain Syndrome?
- Potential Benefits of Diagnosis and Treatment on Health Outcomes Among Elderly People With Symptoms of Overactive Bladder
- The Zika Virus summarised


Great post.
Painful bladder syndrome as defined by the international continence society is, “the presence of suprapubic pain, related while filling of bladder, along with symptoms like urgency in urination in absence of any urinary tract infection.
For more information visit at
https://bit.ly/2JjJFBD
is it possible to import medications for this condition with prescription from USA or AUS?
My gynea wants to use a drug that is not available in NZ and yet as he is american he prescribes the medication regularly in US….
I was diagnosed with IC in mid September. It’s awful, living with it and I can’t see a urologist until Jan. 4th,b/c mhe urologist doesn’t accept my insurance, only Regular Medicare patients! I’m seeing a Nurse Practitioner this week, who accepts my current Medicare Advantage Plan, however. Hope she can help me!